Life Expectancy with Fatty Liver Disease | A Detailed Guide
- What is Fatty Liver Disease?
- What is the life expectancy with fatty liver disease?
- Progression and Complications of Fatty Liver Disease
- Importance of Early Intervention For Fatty Liver Disease
- Alcoholic Fatty Liver Disease (AFLD)
- Risk Factors for Alcoholic Fatty Liver Disease (AFLD)
- Prevention of Alcoholic Fatty Liver Disease (AFLD)
- Nonalcoholic Fatty Liver Disease (NAFLD)
- Risk Factors For Nonalcoholic Fatty Liver Disease (NAFLD)
- Prevention of Nonalcoholic Fatty Liver Disease (NAFLD)
- Impact of Fatty Liver Disease (Both AFLD and NAFLD) on Life Expectancy
- Medical Management and Treatment of Fatty Liver Disease
- Strategies for Managing Fatty Liver Disease
- Resources and Research Studies
- Conclusion
- Frequently Asked Questions (FAQs)
- Citations
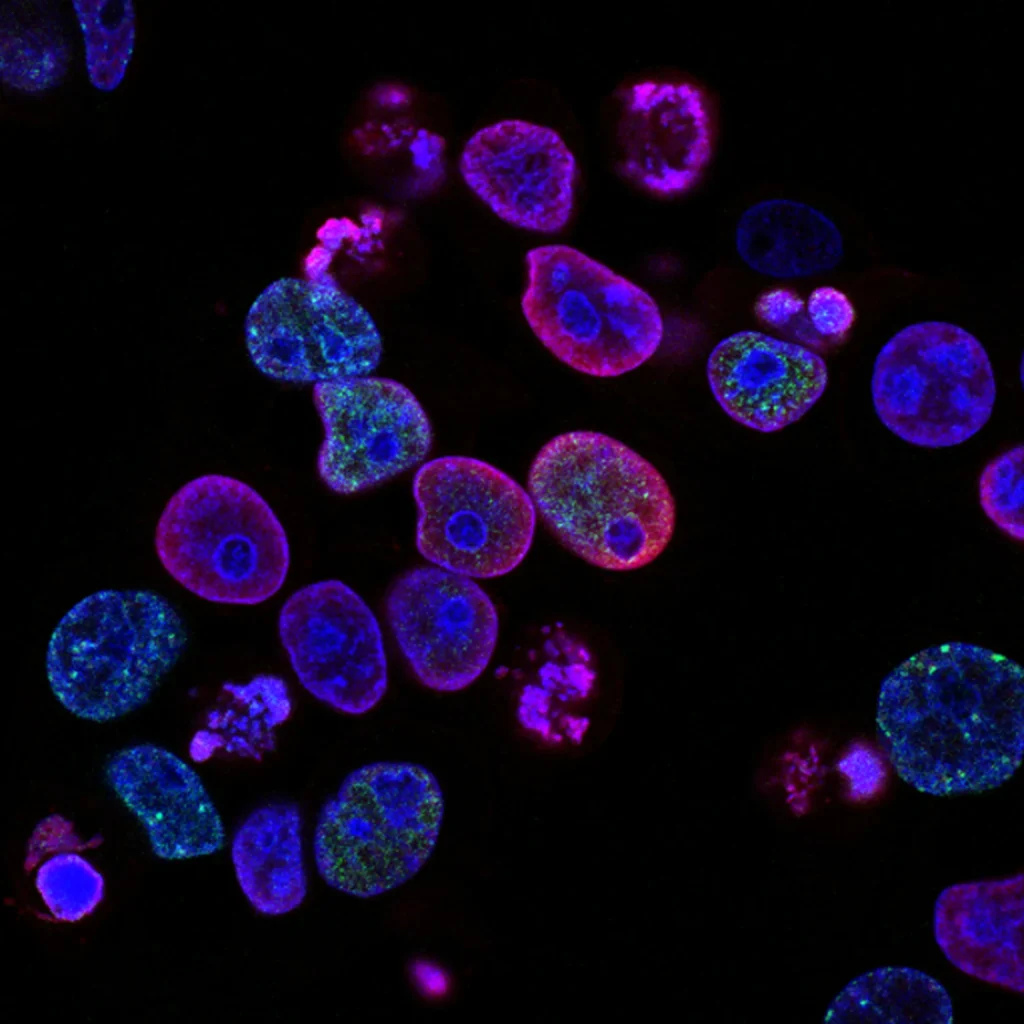
What is Fatty Liver Disease?
This post may contain affiliate links, meaning I may earn a commission if you make a purchase, at no extra cost to you. I only recommend products I trust. Thank you for your support.
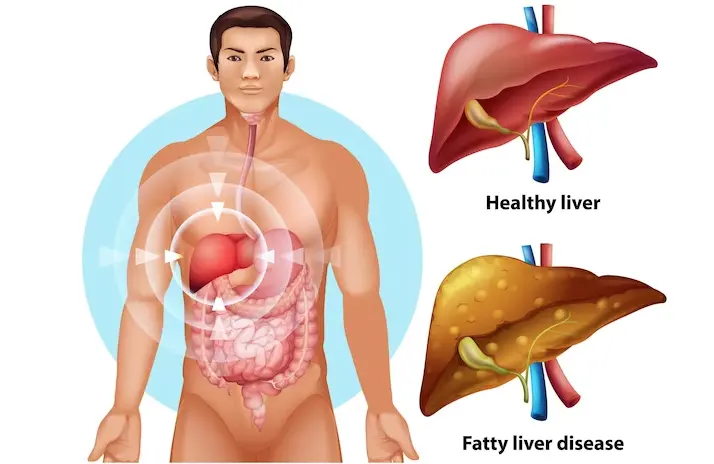
Fatty liver disease, also known as hepatic steatosis, is a condition characterized by the accumulation of fat in the liver. This excessive fat buildup can lead to liver inflammation and impair liver function.
Fatty liver disease can be categorized into two types: Alcoholic Fatty Liver Disease (AFLD) and Non-Alcoholic Fatty Liver Disease (NAFLD).
AFLD is caused by excessive alcohol consumption, while NAFLD is associated with factors such as obesity, insulin resistance, and metabolic syndrome.
Understanding the life expectancy with fatty liver disease is crucial for individuals affected by this condition.
In this article, we shall discuss the risk factors and prevention of fatty liver disease (for both AFLD and NAFLD) to protect ourselves from its harmful effects and promote better liver health.
What is the life expectancy with fatty liver disease?
Life expectancy with fatty liver disease can vary based on disease progression and severity.
In its early stages, fatty liver disease may not cause any symptoms and can be reversible with lifestyle modifications.
However, if left untreated, it can progress to more severe stages, such as liver fibrosis, cirrhosis, and hepatocellular carcinoma.
These advanced conditions potentially cause liver failure and an increased risk of liver cancer.
NAFLD, the most common chronic fatty liver disease across all age groups, affects 14%-30% of the general population due to rising obesity rates.
Nonalcoholic fatty liver disease life expectancy is about 4.2 to 4.4 years for both men and women without a liver transplant.
Advanced stages of the disease, such as cirrhosis, bring complications like swelling, confusion, and gastrointestinal bleeding, further diminishing life expectancy.
Lifestyle choices and understanding risk factors play a key role in reducing the chances of developing severe stages of nonalcoholic fatty liver disease (NAFLD) and its progression to advanced scarring or cirrhosis.
Progression and Complications of Fatty Liver Disease
Fatty liver disease can progress through different stages, each with its own set of complications that can significantly impact an individual’s life expectancy.

Complications associated with advanced stages of fatty liver disease include portal hypertension, esophageal varices, liver failure, and an increased risk of infection.
These complications can further impact life expectancy and overall quality of life.
These stages include:
1. Simple Steatosis
This is the earliest stage of fatty liver disease, characterized by the accumulation of fat in the liver cells. At this stage, there may be no symptoms or noticeable liver damage.
2. Nonalcoholic Steatohepatitis (NASH)
In this stage, inflammation and liver cell damage occur in addition to the accumulation of fat. NASH can lead to more severe complications and is considered a more advanced form of fatty liver disease.
3. Fibrosis
If left untreated, NASH can progress to liver fibrosis, which is the formation of scar tissue in the liver. This can impair liver function and increase the risk of cirrhosis.
4. Cirrhosis
Cirrhosis is a late stage of fatty liver disease characterized by extensive scarring of the liver. It can lead to liver failure and significantly reduce life expectancy.
5. Hepatocellular Carcinoma
In some cases, fatty liver disease can progress to liver cancer, known as hepatocellular carcinoma. This is a life-threatening complication with poor prognosis.
Importance of Early Intervention For Fatty Liver Disease
Early detection, intervention, and lifestyle changes are crucial in improving outcomes and potentially extending individuals’ life expectancy with fatty liver disease.
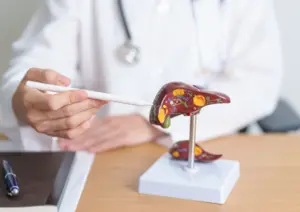
When the disease is diagnosed and managed in its early stages, there is a higher chance of preventing disease progression and reducing the risk of complications.
Early intervention strategies include:
- Regular screenings and check-ups to monitor liver function and detect any changes.
- Lifestyle modifications, including a healthy diet, regular exercise, weight management, and limiting alcohol consumption.
- Medication management for underlying conditions such as diabetes, high cholesterol, and high blood pressure.
- Close collaboration with healthcare providers to develop a personalized treatment plan and address individual needs.
By taking proactive steps and making necessary lifestyle changes, individuals with fatty liver disease can improve their overall health and potentially extend their life expectancy.
Alcoholic Fatty Liver Disease (AFLD)
Alcoholic fatty liver disease (AFLD) is primarily caused by chronic and excessive alcohol consumption, which can overwhelm the liver’s ability to metabolize and process alcohol.
It is the earliest stage of alcohol related liver disease and is characterized by the accumulation of fat in the liver cells.
AFLD can progress to more severe conditions such as alcoholic hepatitis and cirrhosis if alcohol consumption continues.
The following factors contribute to the development of AFLD:
1. Alcohol Consumption
Chronic, heavy alcohol consumption is the primary cause of AFLD. The risk of developing AFLD increases with higher levels and longer durations of alcohol consumption.
2. Metabolism of Alcohol
When the liver metabolizes alcohol, it produces substances that can damage liver cells, leading to the accumulation of fat.
3. Genetic Predisposition
Some individuals may be genetically predisposed to developing AFLD, especially when combined with excessive alcohol intake.
Risk Factors for Alcoholic Fatty Liver Disease (AFLD)
Several factors can increase the risk of developing AFLD:
1. Alcohol Consumption
Chronic and excessive alcohol consumption is the primary risk factor for AFLD.
2. Gender
Women are generally more susceptible to alcohol-related liver damage than men, even with lower levels of alcohol consumption.
3. Genetics
Genetic factors can influence an individual’s susceptibility to AFLD.
4. Obesity
Excessive body weight, especially when combined with heavy alcohol consumption, can increase the risk of developing AFLD.
5. Pre-existing Liver Conditions
Individuals with pre-existing liver conditions may be at a higher risk of developing AFLD when consuming alcohol.
6. Nutritional Factors
Poor nutrition, especially deficiencies in certain nutrients, can exacerbate the effects of alcohol on the liver and increase the risk of AFLD.
Understanding these causes, preventive measures, and risk factors is essential for individuals at risk of AFLD to take proactive steps to protect their liver health and overall well-being.
Prevention of Alcoholic Fatty Liver Disease (AFLD)
Strategies to prevent AFLD include:
1. Moderate Alcohol Consumption
Limiting alcohol intake to moderate levels or abstaining from alcohol altogether is crucial for preventing AFLD. For men, this generally means up to two drinks per day, and for women, up to one drink per day.
2. Seek Support for Alcohol Use
If there are challenges in moderating alcohol consumption, seek support from healthcare professionals or support groups to address alcohol use disorder.
3. Healthy Lifestyle
Adopting a healthy lifestyle, including a balanced diet and regular exercise, can support overall liver health and reduce the risk of developing AFLD.
4. Regular Medical Checkups
Regularly monitor liver health through medical checkups, especially if there is a history of heavy alcohol use or if other risk factors are present.
Nonalcoholic Fatty Liver Disease (NAFLD)
Nonalcoholic fatty liver disease (NAFLD) refers to the accumulation of fat in the liver in individuals who do not consume significant amounts of alcohol.
It encompasses two main types: Nonalcoholic Fatty Liver (NAFL) and Nonalcoholic Steatohepatitis (NASH), each with distinct characteristics and implications.
1. Nonalcoholic Fatty Liver (NAFL)
- Involves the accumulation of fat in the liver without significant inflammation or liver cell damage.
- Often considered relatively benign in its early stages.
- Can progress to a more severe form of the disease, particularly if risk factors are not effectively managed.
2. Nonalcoholic Steatohepatitis (NASH)
- Characterized by liver inflammation and damage in addition to fat accumulation.
- Poses a higher risk of progression to advanced liver disease, including fibrosis, cirrhosis, and liver cancer.
- Associated with an increased risk of cardiovascular disease and other metabolic complications.
- If identified early, individuals with Nonalcoholic Steatohepatitis may offer a live an additional 10 to 15 years.
Risk Factors For Nonalcoholic Fatty Liver Disease (NAFLD)
The following conditions increase the likelihood of developing Nonalcoholic Fatty Liver Disease (NAFLD):
1. Obesity
Excessive body weight is a significant risk factor for the development and progression of NAFLD and NASH.
2. Type 2 Diabetes
Individuals with type 2 diabetes are at a higher risk of developing NAFLD and NASH.
3. Insulin Resistance
Insulin resistance is closely associated with the pathogenesis of NAFLD and NASH.
4. High Cholesterol
Elevated levels of cholesterol contribute to the risk of developing and worsening NAFLD and NASH.
5. Metabolic Syndrome
The presence of metabolic syndrome, characterized by a combination of obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels, increases the risk of NAFLD and NASH.
Prevention of Nonalcoholic Fatty Liver Disease (NAFLD)
Here are some key preventive measures for NAFLD:
1. Healthy Diet
Emphasize a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit intake of added sugars, refined carbohydrates, and saturated fats. Check out the 21 day fatty liver diet plan.
2. Weight Management
Achieve and maintain a healthy weight through a combination of regular physical activity and a balanced diet. Aim for gradual weight loss if overweight or obese.
3. Regular Exercise
Engage in regular physical activity, aiming for at least 150 minutes of moderate-intensity exercise per week.
4. Manage Medical Conditions
Control underlying medical conditions such as obesity, type 2 diabetes, high cholesterol, and metabolic syndrome through lifestyle changes and, if necessary, medication.
5. Limit Alcohol Consumption
Even though NAFLD is not caused by alcohol, excessive alcohol consumption can worsen liver health. Therefore, limiting alcohol intake is advisable.
6. Avoiding Unnecessary Medications
Use medications, especially over-the-counter drugs and supplements, under the guidance of a healthcare professional to avoid unnecessary stress on the liver.
Impact of Fatty Liver Disease (Both AFLD and NAFLD) on Life Expectancy
Fatty Liver Disease can have a significant impact on life expectancy if left untreated or not addressed promptly.
Some of these impacts include:
1. Cirrhosis
- Advanced scarring of the liver can lead to liver failure and other serious complications.
- Significantly reduces life expectancy due to the potential for liver failure and other serious complications.
- Increases the risk of mortality, especially if complications such as esophageal varices or hepatic encephalopathy develop.
- May necessitate liver transplantation, which can impact life expectancy and overall health outcomes.
2. Liver Cancer
- AFLD and NAFLD are associated with an increased risk of developing liver cancer.
- Increases the risk of mortality, especially in advanced stages of liver cancer.
- Often associated with poor prognosis, potentially leading to a significant reduction in life expectancy.
- Requires aggressive treatment approaches, which can impact quality of life and overall survival.
3. Cardiovascular Disease
- Both AFLD and NAFLD are linked to an elevated risk of cardiovascular complications, including heart disease and stroke.
- Contributes to a decrease in life expectancy due to the potential for major adverse cardiovascular events.
- Requires comprehensive management to mitigate the impact on life expectancy and overall health outcomes.
Medical Management and Treatment of Fatty Liver Disease
Medical management and treatment play a crucial role in mitigating the impact of fatty liver disease on life expectancy.
It is important to consult with healthcare providers for personalized advice and management of fatty liver disease.
They can provide guidance on appropriate treatment options, lifestyle modifications, and regular monitoring to optimize outcomes and potentially extend life expectancy.
Treatment options for fatty liver disease include:
1. Medications
Certain medications, such as vitamin E and pioglitazone, may be prescribed to manage the underlying conditions associated with fatty liver disease and reduce liver inflammation.
2. Weight Loss
Losing weight through a combination of weight loss diet plans and physical exercises is an essential component of managing fatty liver disease. Weight loss can help reduce liver fat and improve liver function.
3. Insulin Sensitizers
Insulin sensitizers, such as metformin, may be prescribed to improve insulin resistance and manage diabetes, which can contribute to fatty liver disease.
4. Regular Monitoring
Regular liver function tests and imaging studies, such as ultrasound or MRI, can help monitor disease progression and guide treatment decisions.
5. Liver Transplantation
In severe cases of liver cirrhosis or liver failure, liver transplantation may be necessary to improve life expectancy. This is a complex procedure and requires careful evaluation and consideration by a specialized medical team.
Strategies for Managing Fatty Liver Disease
Fatty liver disease can have a significant impact on an individual’s overall quality of life.
The presence of symptoms, disease progression, and the potential for complications can affect daily activities, emotional well-being, and social interactions.
However, there are strategies to manage symptoms and optimize well-being:
1. Symptom Management
Managing symptoms such as fatigue, abdominal pain, and jaundice can improve quality of life. This may involve medication, dietary modifications, and lifestyle changes.
2. Emotional Support
Seeking emotional support from family, friends, or support groups can help individuals cope with the challenges of living with fatty liver disease. Professional counseling may also be beneficial.
3. Healthy Lifestyle
Adopting a healthy lifestyle that includes regular exercise, stress management techniques, and a balanced diet can improve overall well-being and reduce the impact of fatty liver disease.
4. Managing Comorbidities
Proper management of underlying conditions such as diabetes, obesity, and high blood pressure can improve quality of life and reduce the risk of fatty disease progression.
Resources and Research Studies
Here are some resources where you can find more information and support:
- American Liver Foundation
- National Institute of Diabetes and Digestive and Kidney Diseases
- American Association for the Study of Liver Diseases
- Long term follow-up and liver-related death rate in patients with non-alcoholic and alcoholic related fatty liver disease
Remember, early detection and intervention are key to improving outcomes and potentially extending life expectancy for individuals with fatty liver disease.
Do not hesitate to reach out to healthcare professionals for guidance and support.
Conclusion
Fatty liver disease is a common condition that can have a significant impact on life expectancy if left untreated.
While individuals with NAFLD generally have a normal life expectancy, those with NASH and advanced stages of the disease may be at a higher risk of complications that can shorten life expectancy.
However, early intervention, lifestyle modifications, and regular monitoring can help slow down disease progression and improve outcomes.
Understanding the causes, risk factors, and symptoms of fatty liver disease is crucial for early diagnosis and intervention.
Adhering to treatment plans, adopting a healthy lifestyle, and seeking support from healthcare professionals and support groups can improve life expectancy and overall quality of life.
It is important to remember that each individual’s journey with fatty liver disease is unique, and proactive management is key to optimizing outcomes.
By taking control of your health and making informed decisions, you can improve our chances of living a long and healthy life.
If you or a loved one has been diagnosed with fatty liver disease, it is essential to seek professional guidance for personalized advice, regular screenings, and comprehensive management.
Healthcare providers, such as hepatologists and gastroenterologists, specialize in liver diseases and can provide expert care and guidance.
In summary, the life expectancy with fatty liver disease varies based on the progression and severity of the condition.
Check out these articles for a healthy nutrition:
- 7-day meal plan for prediabetes
- Friendly diabetic meal plan
- 7-day meal plan for gestational diabetes
- 7-day meal plan for ulcerative colitis
- 7-day meal plan for gastritis
- South beach diet for weight loss
- Nurse Anesthetist salary
- 7-day carb cycling meal plan
- Beginner intermittent fasting meal plan
- 7-day Daniel Fast meal plan
Frequently Asked Questions (FAQs)
Can fatty liver disease be reversed?
Yes, fatty liver disease can be reversed, especially in its early stages. Lifestyle modifications, including weight loss, a healthy diet, regular exercise, and alcohol limitation, can help reduce liver fat and improve liver function.
However, in more advanced stages, such as cirrhosis, the damage may be irreversible.
What are the symptoms of fatty liver disease?
Fatty liver disease may not cause any symptoms in its early stages. However, as the disease progresses, symptoms may include fatigue, abdominal pain, jaundice (yellowing of the skin and eyes), and swelling in the legs and abdomen.
Can fatty liver disease shorten your life expectancy?
Yes, fatty liver disease can potentially shorten life expectancy, especially if it progresses to more severe stages such as non-alcoholic steatohepatitis (NASH) or cirrhosis by 3 to 5 years.
How does age and gender influence life expectancy in individuals with fatty liver disease?
Older age and male gender are associated with a higher risk of fatty liver disease progression and complications, which can affect life expectancy.
Can fatty liver disease lead to liver cancer?
Yes, fatty liver disease, especially in its more severe form (NASH), can increase the risk of developing liver cancer, known as hepatocellular carcinoma.
Citations
- Thandra KC, Barsouk A, Saginala K, Aluru JS, Rawla P, Barsouk A. Epidemiology of non-alcoholic fatty liver disease and risk of hepatocellular carcinoma progression. Clin Exp Hepatol. 2020 Dec;6(4):289-294. doi: 10.5114/ceh.2020.102153. Epub 2020 Dec 30. PMID: 33511275; PMCID: PMC7816638.
- Abd El-Kader SM, El-Den Ashmawy EM. Non-alcoholic fatty liver disease: The diagnosis and management. World J Hepatol. 2015 Apr 28;7(6):846-58. doi: 10.4254/wjh.v7.i6.846. PMID: 25937862; PMCID: PMC4411527.