What Is Celiac Disease? A Comprehensive Guide
- What is Celiac Disease?
- Is Celiac Disease Hereditary?
- Symptoms of Celiac Disease
- What Happens if You Leave Celiac Disease Untreated?
- Diagnosis and Testing
- Complications of Untreated Celiac Disease
- How to Treat Celiac Disease With a Gluten Free Diet
- 7-Day Gluten Free Diet for Celiac Disease
- Living Well with Celiac Disease
- Living Well with Celiac Disease
This post may contain affiliate links, meaning I may earn a commission if you make a purchase, at no extra cost to you. I only recommend products I trust. Thank you for your support.
Discovering you have celiac disease can turn your world upside down, forcing you to rethink everything about your diet and health.
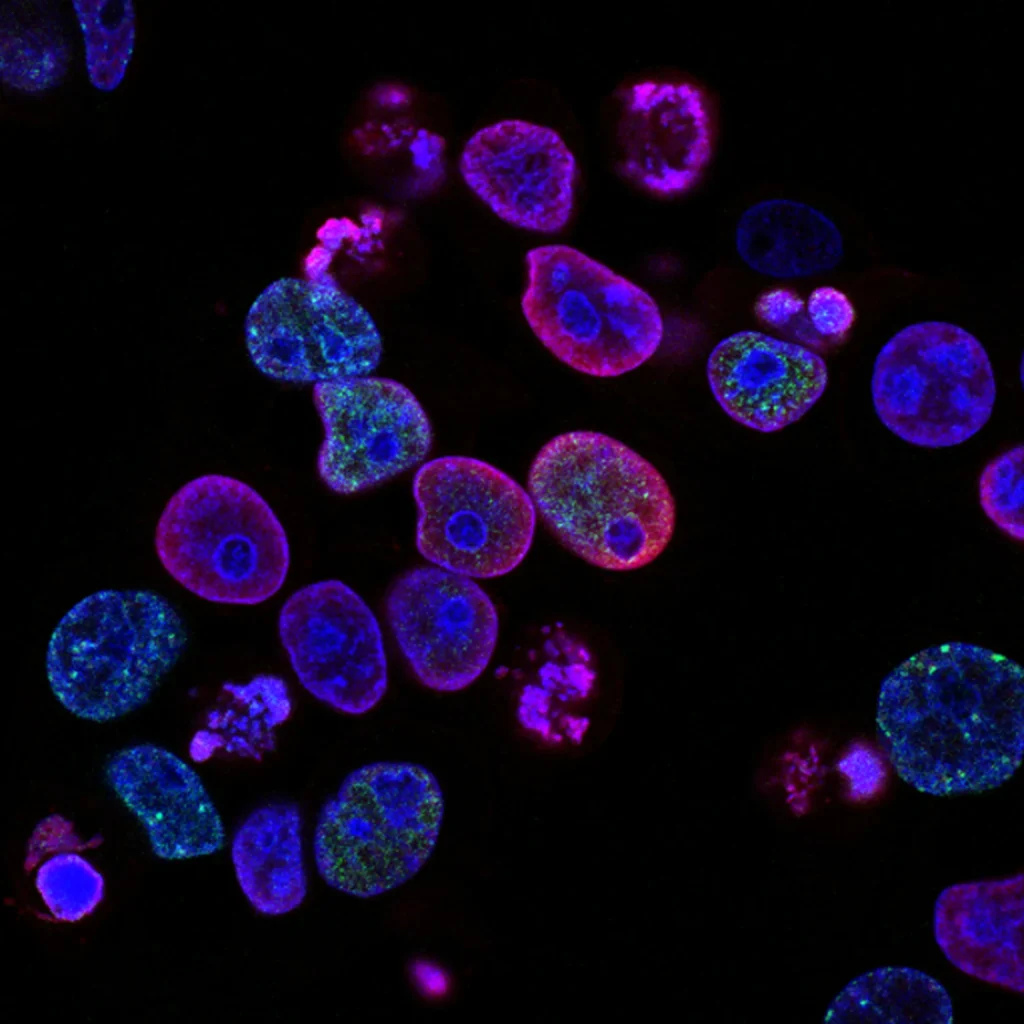
Gastrointestinal infections are among the environmental factors that may contribute to the development of celiac disease in genetically predisposed individuals.
This serious autoimmune disorder affects 1 in 100 people worldwide, triggering harmful immune responses when gluten is consumed.
The body mistakenly attacks its own tissues, damaging the small intestine and preventing proper nutrient absorption.
Left untreated, celiac disease can lead to severe complications including malnutrition, osteoporosis, and even certain cancers.
Understanding this condition is crucial for proper diagnosis, effective management, and living a healthy, symptom-free life.
What is Celiac Disease?
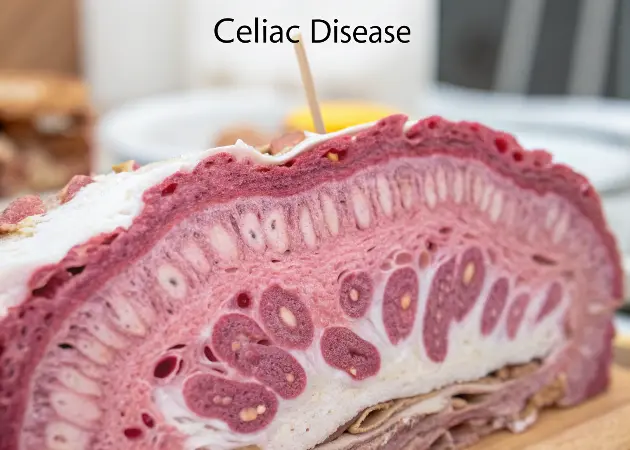
Celiac disease is a serious autoimmune disorder where consuming gluten causes your immune system to attack your small intestine. Celiac disease is also known as gluten-sensitive enteropathy.
Gluten, a protein found in wheat, barley, and rye, triggers this abnormal response that damages the villi, small, finger-like projections lining your small intestine.
These villi are essential for absorbing nutrients from food.
When damaged, your body cannot properly absorb nutrients, including vitamins, minerals, and other essential nutrients, leading to malnutrition despite eating a balanced diet.
This malabsorption can affect virtually every system in your body, from your bones to your brain, making celiac disease much more than just a digestive disorder.
Inflammatory cells are sent to the small intestine to destroy gluten molecules, leading to further damage.
Unlike food allergies that cause immediate reactions, celiac damage occurs slowly over time, making it particularly dangerous when undiagnosed.
Immune cells are activated to attack gluten, causing further damage to the mucosa.
Is Celiac Disease Hereditary?
- Celiac disease runs strongly in families, with first-degree relatives (parents, siblings, children) having a 1 in 10 risk of developing celiac disease compared to 1 in 100 in the general population
- Nearly 97% of people with celiac disease carry specific genetic markers called HLA-DQ2 or HLA-DQ8, though having these genes doesn’t guarantee developing the disease
- People of Northern European descent face higher rates, with approximately 1% of European and North American populations affected
- Women are diagnosed with celiac disease at least twice as often as men, showing a significant gender disparity
- Individuals with chromosomal disorders including Down syndrome, Turner syndrome, and Williams syndrome have substantially higher rates of celiac disease
- Having other autoimmune conditions significantly increases risk, particularly Type 1 diabetes, autoimmune thyroid disease, rheumatoid arthritis, and microscopic colitis
- Environmental triggers appear necessary to activate the disease in genetically susceptible people, including surgery, pregnancy, viral infections, or severe emotional stress
- Two common onset windows exist: early childhood (8-12 months) when gluten is first introduced, and mid-life (40-60 years) when other health factors may trigger the condition. Risk factors such as genetic predispositions and other health disorders play a crucial role in the development of celiac disease.
Symptoms of Celiac Disease
1. Digestive Symptoms
The most recognizable signs of celiac disease are gastrointestinal symptoms that affect the digestive system.
Eating foods containing gluten can trigger these symptoms. Many patients experience chronic diarrhea or constipation that doesn’t respond to standard treatments.
Abdominal pain and bloating often occur after consuming gluten-containing foods, sometimes accompanied by loud stomach gurgling. Gas, nausea, and vomiting can become common occurrences.
A particularly telling sign is fatty, pale, and foul-smelling stools (steatorrhea), indicating that fats aren’t being properly absorbed due to intestinal damage.
2. Non-Digestive Symptoms
What makes celiac disease particularly challenging to diagnose is that over half of affected adults experience symptoms unrelated to the digestive system.
Unexplained fatigue and weakness often result from iron-deficiency anemia, as iron absorption is compromised.
Many patients develop bone or joint pain due to calcium malabsorption. Untreated celiac disease can lead to significant weight loss due to the inability of the damaged intestines to effectively absorb nutrients.
Depression, anxiety, and “brain fog” can stem from nutritional deficiencies or inflammation. Some develop peripheral neuropathy (tingling in hands and feet), unexplained seizures, or migraines.
Skin conditions like dermatitis herpetiformis an intensely itchy, blistering rash appears in about 25% of patients.
Additionally, the impairment of nutrient absorption resulting from villous atrophy may lead to a decreased production of lactase, the enzyme necessary for digesting lactose, thereby resulting in lactose intolerance which typically resolves after treatment of celiac disease.
3. Symptoms in Children
Children with celiac disease often show distinctly different symptoms than adults.
Failure to thrive and unexplained growth delays are major red flags in pediatric cases.
Many children develop short stature or experience delayed puberty due to nutritional deficiencies.
Neurological symptoms can include attention and learning deficits, which may be misdiagnosed as behavioral problems.
Irritability is extremely common, as children can’t articulate their discomfort.
Dental enamel defects, including pitting and discoloration, can provide visual clues to malabsorption during tooth development.
Gluten sensitivity can cause similar symptoms in children, even though it does not involve the same immune response or intestinal damage as celiac disease.
Eating gluten can trigger these symptoms in children, leading to various health issues and complications.
What Happens if You Leave Celiac Disease Untreated?
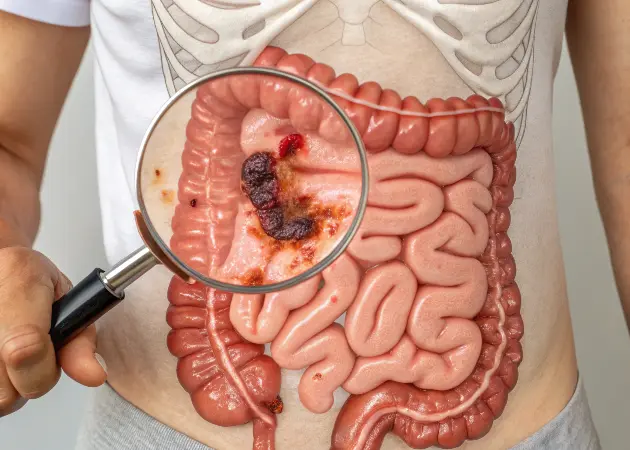
Leaving celiac disease untreated creates a dangerous cycle of progressive intestinal damage and worsening health.
Untreated celiac disease can lead to developing complications such as cancers and other significant gastrointestinal problems.
Initially, you might experience fatigue, digestive discomfort, and nutritional deficiencies that seem manageable.
Over time, however, the chronic inflammation and malabsorption lead to serious complications and your risk of developing additional autoimmune diseases rises significantly.
Studies show that diagnosis after age 20 increases the chance of developing another autoimmune condition to 34%, compared to just 10.5% when diagnosed before age 4.
The intestinal lining becomes increasingly damaged, making recovery more difficult and potentially leading to refractory celiac disease that doesn’t respond well to treatment.
Untreated celiac disease also carries a slightly increased risk of early death and cancers such as intestinal lymphoma.
Diagnosis and Testing
1. Blood Testing
Blood tests serve as the primary screening tool for diagnosing celiac disease, measuring the body’s immune response to gluten.
The most sensitive and specific test looks for tissue transglutaminase antibodies (tTG-IgA), which are elevated in most people with active celiac disease.
Other helpful tests include endomysial antibody (EMA) and deamidated gliadin peptide (DGP) antibodies.
Importantly, these tests are only reliable if you’re currently consuming gluten. If you’ve already adopted a gluten-free diet, you may need to undergo a gluten challenge before testing.
Some doctors also order genetic testing for HLA-DQ2 and HLA-DQ8 markers, which can help rule out celiac disease if negative.
Guidelines from the national institute, such as the National Institute for Health and Clinical Excellence (NICE) in England, recommend specific protocols for screening and diagnosing celiac disease.
2. Intestinal Biopsy
The gold standard for diagnosing celiac disease remains an upper endoscopy with small intestine biopsy.
During this procedure, a gastroenterologist passes a thin, flexible tube with a camera (endoscope) through your mouth, stomach, and into the first part of your small intestine (duodenum).
They collect several tiny tissue samples to examine under a microscope, looking for characteristic signs of damage to the intestinal wall, including flattened villi, increased lymphocytes, and crypt hyperplasia.
Multiple samples are taken because damage can be patchy, especially in early disease.
This procedure typically takes less than 30 minutes and is performed under sedation to ensure comfort.
3. Nutritional Assessment
Once diagnosed, comprehensive nutritional testing helps identify specific deficiencies caused by the small intestine’s inability to absorb nutrients effectively.
These nutritional deficiencies are commonly identified through tests such as complete blood count, iron studies, vitamin B12, folate, vitamin D, calcium, and liver function.
Many newly diagnosed patients show significant deficiencies that require targeted supplementation.
Bone density scans are recommended for adults to check for osteopenia or osteoporosis resulting from calcium and vitamin D malabsorption.
Your doctor may also screen for associated conditions like thyroid disorders, Type 1 diabetes, and liver abnormalities, which commonly co-occur with celiac disease.
Complications of Untreated Celiac Disease
Untreated celiac disease progressively damages the small intestine, creating far-reaching health problems beyond digestive symptoms.
Chronic malnutrition leads to bone density loss, with over 70% of untreated patients developing osteopenia or osteoporosis.
Neurological complications affect up to 22% of patients, including peripheral neuropathy, balance problems, and even seizures.
Women face increased rates of infertility, miscarriage, and pregnancy complications.
The longer celiac disease remains untreated, the greater the risk of serious complications.
Intestinal damage increases the chance of developing small intestine cancer by 60-80 times compared to the general population.
Lymphoma risk also rises significantly. Liver abnormalities occur in up to 40% of patients, potentially progressing to severe liver disease.
Untreated celiac disease can also lead to the development of multiple sclerosis, highlighting the severe health implications.
The longer celiac disease goes untreated, the greater the risk of developing additional autoimmune conditions. Research shows that the risk increases with age at diagnosis:
- Diagnosed between ages 2–4: 10.5% risk
- Diagnosed between ages 4–12: 16.7% risk
- Diagnosed between ages 12–20: 27% risk
- Diagnosed after age 20: 34% risk
The inflammatory burden from untreated celiac disease significantly impacts quality of life comparable to the treatment burden experienced by individuals with end-stage renal disease.
Moreover, untreated celiac disease raises the likelihood of developing other autoimmune disorders such as type 1 diabetes and multiple sclerosis.
How to Treat Celiac Disease With a Gluten Free Diet
The only effective treatment for celiac disease is strict, lifelong adherence to a strict gluten free diet.
This means eliminating all forms of wheat, barley, and rye from your meals and snacks.
Even trace amounts of gluten as little as 1/8 teaspoon of flour can trigger intestinal damage in sensitive individuals.
Gluten exposure can have detrimental effects on individuals with celiac disease, leading to symptoms and complications.
Obvious sources of gluten include bread, pasta, cereals, and baked goods made with wheat flour.
However, gluten hides in many unexpected places: soy sauce, salad dressings, processed meats, medications, and even some supplements.
Learning to read labels for hidden gluten becomes essential, as does understanding cross-contamination risks when preparing food.
It is also important to avoid processed foods that may contain hidden gluten, as they can be a source of contamination.
Most patients experience symptom improvement within weeks of eliminating gluten, though complete intestinal healing may take months to years, especially in adults with longstanding disease.

7-Day Gluten Free Diet for Celiac Disease
This 7-day gluten free meal plan completely eliminates all sources of gluten, including even small traces that can cause intestinal damage in people with celiac disease.
This celiac disease diet features gluten free foods such as:
- Fruits and vegetables
- Meat, poultry, and fish (unbreaded and unprocessed)
- Eggs
- Dairy products (check labels for additives)
- Beans, legumes, and nuts
- Gluten-free grains (rice, quinoa, buckwheat, corn, millet, amaranth, gluten free oats)
| Day | Breakfast | Lunch | Dinner | Snacks |
| Monday | Quinoa breakfast bowl with berries, sliced almonds, and cinnamon | Grilled chicken salad with mixed greens, cherry tomatoes, cucumbers, and olive oil vinaigrette | Baked salmon with roasted sweet potatoes and steamed broccoli | Plain Greek yogurt with honey; Rice cakes with almond butter |
| Tuesday | Smoothie with banana, spinach, almond milk, and certified gluten-free protein powder | Mexican bowl with corn tortillas, black beans, brown rice, avocado, and salsa | Turkey meatballs with zucchini noodles and marinara sauce (check for gluten-free) | Apple slices with cheddar cheese; Mixed nuts |
| Wednesday | Gluten-free oatmeal with chia seeds, blueberries, and maple syrup | Tuna salad (made with gluten-free mayonnaise) on corn tortillas with lettuce | Stir-fried beef with rice noodles, bell peppers, snap peas, and gluten-free tamari sauce | Carrot sticks with hummus; Orange slices |
| Thursday | Scrambled eggs with spinach, feta cheese, and cherry tomatoes | Quinoa bowl with roasted vegetables, chickpeas, and tahini dressing | Grilled pork chops with mashed potatoes and green beans | Rice crackers with avocado; Strawberries |
| Friday | Chia pudding with coconut milk, vanilla, and fresh fruit | Leftover pork with mixed green salad and balsamic vinaigrette | Baked chicken thighs with wild rice and roasted Brussels sprouts | Gluten-free energy bar; Pear |
| Saturday | Gluten-free pancakes topped with banana slices and pure maple syrup | Lentil soup with gluten-free bread | Shrimp and vegetable skewers with quinoa | Popcorn (plain); Grapes |
| Sunday | Vegetable frittata with potatoes and herbs | Gluten-free sandwich with turkey, lettuce, tomato, and avocado on gluten-free bread | Pot roast with carrots, potatoes, and celery | Dark chocolate squares; Mixed berries |
Important Notes:
- Always check labels for hidden gluten in packaged foods
- Use dedicated cutting boards and utensils to prevent cross-contamination
- Focus on naturally whole gluten free foods when possible
- Adapt portion sizes based on individual caloric needs
- Consult with a registered dietitian for personalized recommendations
Living Well with Celiac Disease
1. Managing Your Kitchen and Home
Creating a safe food environment with gluten free foods is fundamental to successfully managing celiac disease.
Many families choose to maintain a completely gluten-free kitchen to eliminate cross-contamination risks.
If this isn’t possible, designate separate preparation areas, cooking utensils, and storage spaces for gluten-free items.
Toasters, colanders, and wooden cutting boards are particularly prone to harboring gluten particles and should be kept separate or replaced with dedicated gluten-free versions.
Label all condiments that might be contaminated by double-dipping, such as butter, mayonnaise, and peanut butter.
Consider color-coding kitchen tools for easy identification.
Regular cleaning of all kitchen surfaces helps prevent accidental exposure, as does handwashing after handling gluten-containing foods.
2. Navigating Social Situations and Dining Out
Social gatherings and restaurant meals present unique challenges, but shouldn’t prevent you from enjoying an active social life.
With a little planning and communication, you can participate confidently and safely.
When dining out, do your homework ahead of time. Look for restaurants with gluten-free menus or a reputation for accommodating special dietary needs.
Call during non-peak hours to speak with the staff and explain your dietary requirements. When ordering, use clear, polite phrases like:
- “Do you have a separate preparation area for gluten-free meals?”
- “Are your fryers dedicated gluten-free?”
It is crucial to avoid eating gluten to prevent triggering an immune response that can damage the small intestine and lead to various symptoms and complications.
For parties and family gatherings, offer to bring a dish you know is safe. Consider eating a small meal beforehand if you’re uncertain about food options.
Educate close friends and family about cross-contamination risks while remaining positive most people want to support your health once they understand the importance.
3. Maintaining Nutritional Balance
A gluten free diet for celiac disease requires careful planning to ensure nutritional adequacy and to help the body absorb nutrients effectively.
Many gluten free foods are lower in fiber, iron, and B vitamins than their gluten-containing counterparts.
Focus on whole gluten free foods like fruits, vegetables, unprocessed meats, fish, legumes, and gluten-free grains such as rice, quinoa, and certified gluten-free oats.
Nutritional deficiencies need to be addressed to prevent health complications.
Work with a registered dietitian who specializes in celiac disease to develop a balanced meal plan.
Most newly diagnosed patients benefit from supplements to correct existing deficiencies, particularly iron, calcium, vitamin D, and B vitamins.
Regular blood work helps monitor nutritional status and guides supplementation needs.
4. Finding Support and Resources
Connecting with others who understand the challenges of celiac disease provides invaluable emotional and practical support.
National organizations like the Celiac Disease Foundation offer reliable information, physician directories, and community forums.
The National Institute for Health and Clinical Excellence (NICE) provides guidelines for screening and diagnosing celiac disease, ensuring standardized care.
Many hospitals with celiac centers offer educational programs and dietitian services.
Smartphone apps can help identify gluten-free products and restaurants while traveling.
Mental health support is also important, as adjusting to the diagnosis and lifestyle changes can sometimes trigger anxiety or depression.
Living Well with Celiac Disease
Celiac disease presents significant challenges, but with proper management, affected individuals can lead full, healthy lives.
Strict adherence to a gluten-free diet remains the cornerstone of treatment, allowing intestinal healing and symptom relief.
Regular medical follow-ups, nutritional counseling, and connection with support groups provide essential resources for long-term success.
While researchers continue exploring potential treatments beyond dietary management, today’s improved diagnostic methods and growing awareness mean more people receive proper care earlier.
With vigilance and support, those with celiac disease can effectively control their condition and thrive despite its challenges.